Anorectal Abscess
An anorectal (perianal) abscess is a collection of pus near the anus, and a common reason for admission to hospital worldwide. Anorectal abscesses tend to be more common in people aged 20–30 years, but can occur at any age. They seem to affect men twice as often as women.
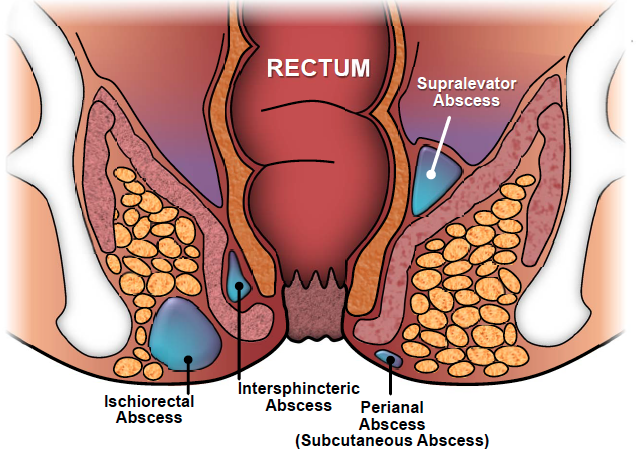
The anal canal is surrounded by the anal sphincter, which helps to keep people continent of faeces. The anal sphincter is made up of two sets of circular muscles and in between them are the anal glands, also known as the anal crypts. These glands produce secretions that enter the anus by crossing the inner ring of muscles.
Ninety percent of all infections in the anorectal area are due to an abscess forming in an anal gland. The remaining 10% of anorectal infections have rarer causes, such as Crohn’s disease or hidradenitis suppurativa (an inflammatory skin condition), trauma, or occasionally cancer.
Most people with an anorectal abscess complain of a pain around the anus, which can be dull or throbbing, and is particularly painful on sitting down. Other people notice a discharge or swelling in the painful area, and may develop a fever. The pain usually increases in intensity until the abscess spontaneously discharges or is treated surgically.
Diagnosis
Most abscesses can be seen directly, so are easily diagnosed by a specialist. Sometimes a computed tomography (CT) or magnetic resonance imaging (MRI) scan of the pelvis is needed to diagnose deep-seated infections, which do not have the typical skin changes. These scans may also help in diagnosing the rarer causes of an anorectal abscess. Occasionally an examination under general anaesthesia in the operating theatre is needed to make the diagnosis, in which case the abscess is treated at the same time.
Treatment
If caught early by the GP, an anorectal abscess can be treated successfully with antibiotics alone. However, if pain and signs of infection increase, an urgent referral to a specialist is needed. Nearly all people in this situation need abscess incision and drainage. After surgery, the wound is left open to allow the pus to continue to drain. Over the next few weeks, the wound heals slowly from the inside out.
Antibiotics are rarely required for an anorectal abscess that has been drained surgically. The exceptions are when an abscess occurs in a diabetic patient or if the surrounding skin is very inflamed and infected. Antibiotics do not to help heal the wound, they merely help to tackle the infection associated with it.
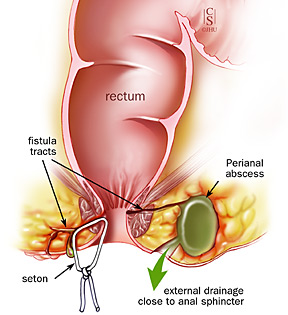
Two thirds of people with an anorectal abscess will never have the problem again after surgery. However, the remaining third will go on to have further problems, which are likely to include developing a new abscess or forming a fistula, which is an abnormal connection between the inside of the anus and the outside of the skin, and also requires surgical treatment.
For more information on anal abscesses, please visit http://patient.info/doctor/anorectal-abscess

