- Abscess Incision and Drainage
- Advancement Flap Repair
- Anal Bulking
- Anal Tattooing
- Botulinum Toxin Injection
- Colectomy
- Delorme’s Procedure
- ELAPE Procedure
- Femoral Hernia Repair
- Fistulotomy
- Haemorrhoidectomy
- HALO-RAR Procedure
- Inguinal Hernia Repair
- Intersphincteric APR
- Lateral Internal Sphincterotomy
- Low Anterior Resection
- Pelvic Organ Prolapse
- Perineal Rectosigmoidectomy
- Rectoanal Repair
- Rubber Band Ligation
- Stapled Haemorrhoidopexy
- Stoma Creation
- Stoma Reversal
- Transanal Rectocoele Repair
- Umbilical Hernia Repair
Stapled Haemorrhoidopexy
Stapled haemorrhoidopexy is a relatively new technique and a significant advance in the treatment of large internal haemorrhoids. Using this procedure, the surgeon can remove haemorrhoidal tissue and “staple” the loose supporting tissue that allows the haemorrhoids to drop down and protrude, returning them to their normal position. The incision is made in the anal canal above the dentate line, so there are no painful external wounds after surgery. You will have the opportunity to discuss fully all the risks and benefits of the operation with me before signing your consent form.
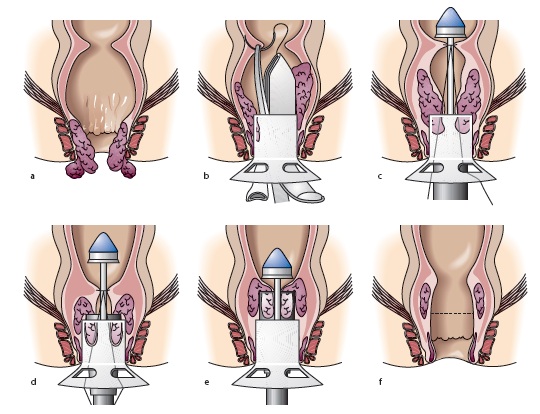
Performed as an open procedure, a circular hollow tube (proctoscope) is first inserted into the anal canal. A long thread (suture) is passed through the tube and stitched in a circle above the internal haemorrhoids. The stapler (an instrument with a circular stapling device at the end) is advanced through the hollow tube and the ends of the thread are pulled. Tightening the thread pulls the loose supporting haemorrhoidal tissue into the jaws of the stapling device. The haemorrhoidal cushions are then pulled back up into their normal position inside the anal canal. When the stapler is fired, it cuts off the ring of expanded haemorrhoidal tissue trapped within the stapler and staples together the upper and lower edges of the cut tissue, at the same time disrupting the blood supply to the haemorrhoids. The whole procedure takes about 30 minutes.
A stapled haemorrhoidopexy is done as a day-stay procedure under general anaesthesia. You will need to fast from midnight on the night before if your surgery is scheduled for the morning, or from 7 am if it scheduled for the afternoon.
No special bowel preparation is necessary before your procedure, unless you are also having a colonoscopy in the same sitting. You will receive an enema one hour or so before your surgery. You will be given a long-acting antibiotic in the anaesthetic room and an injection of local anaesthetic before you leave the operating theatre.
After the operation you will be transferred to the recovery area and then to the ward. You should be able to go home the same day, but sometimes patients may need to stay longer. You should not drive after your surgery, so a friend or relative will need to take you home.
Some discomfort is common after surgery when your local anaesthetic wears off. This will get better, but may take 4–6 weeks to resolve completely. It is important to keep your bowel movements soft and regular during this time. To prevent constipation, eat foods high in fibre, and drink plenty of water (6–8 glasses a day). Analgesia, laxatives and a 5-day course of antibiotics will be given to you to take home. It is best to keep up with the analgesia and laxatives until your bowels are moving and any discomfort is manageable. Laxatives may need to be continued for up to one month after surgery.
You can expect minor bleeding after this procedure, and a sanitary towel changed twice daily will help to prevent staining of underwear. It is normal to notice a small amount of bleeding after you have opened your bowels, but if the amount of blood is more than a couple of teaspoons a day, please let my office know.
Patients are usually able to resume all normal activities, including going back to work, 1–2 weeks after surgery. Exactly when patients can resume driving after this type of surgery is determined on a case-by-case basis. This is usually 1–2 weeks, and will be discussed with you after your surgery. Please let your insurance company know when you have been given the all-clear to resume driving.
People who undergo a stapled procedure for their haemorrhoids tend to have less pain after surgery than those who undergo traditional haemorrhoid surgery. However, the long-term success rate for a stapled procedure is less than for conventional haemorrhoidectomy. Generally, larger prolapsing haemorrhoids are best treated by a conventional technique.
A follow-up appointment in the clinic will be arranged 1–2 weeks after your surgery to check that your symptoms have resolved and discuss any further management if required.

