Pelvic Organ Prolapse
The pelvic floor consists of a group of muscles together with fascia, ligaments, and tendons that keep the pelvic organs and structures, i.e., the bladder, uterus (in women), and rectum in their correct place. These muscles also help to control the release of faeces from the rectum and urine from the urethra, so need to be strong to maintain continence as well as be flexible and able to relax when we go to the toilet.
When the muscles of the pelvic floor or their surrounding structures become weakened, damaged or uncoordinated, they may no longer be able to support the weight of one or more of the pelvic organs. When this happens, a pelvic floor organ may drop down from its normal position. This is known as pelvic organ prolapse. In some cases, the pelvic floor itself may prolapse as well.
Women are more prone to pelvic floor dysfunction than men, the most common cause being damage to the pelvic floor during childbirth, particularly if the second stage of labour is prolonged, the baby’s head is in an unusual position, or forceps are needed. Muscle mass tends to start decreasing at around 40 years of age, and if there is pre-existing damage to the pelvic floor, pelvic floor dysfunction may start to become apparent at this time. After the menopause, further muscle mass is lost, and some of the connective tissues may start to lose their strength, further weakening the pelvic floor. However, there are other causes of pelvic organ dysfunction and prolapse, and some women who have never had children (and men) suffer from pelvic floor dysfunction. Ongoing constipation and straining when going to the toilet also increase the risk of pelvic organ prolapse.
As with many other conditions, there is a genetic component to pelvic organ prolapse. Most people receive genes from their parents that provide a good balance between strength, flexibility and coordination in the pelvic floor. However, some people are born with more elastic connective tissues that stretch easily with age. A minority of people are born with a condition known as hypermobility syndrome, in which the connective tissues are markedly weak. These people tend to be double-jointed, very flexible, and athletic in younger adulthood, but the pelvic floor in these individuals may become weaker over time, leading to pelvic floor dysfunction.
When the pelvic floor starts to prolapse, stretching of the pelvic ligaments may result in a dragging pelvic sensation. This occurs only on standing up, and when the effect of gravity is removed by lying down, the dragging sensation ceases. Any trauma or tear in the muscle can lead to trigger points. These are similar to knots found in other muscles. These trigger points can cause muscles to act in an abnormal fashion and be painful to touch. Intercourse and the need to go to the toilet can trigger these pains, and treatment is generally needed to restore correct functioning of the pelvic floor.
The most common types of prolapse seen by a colorectal surgeon are those involving the rectum, vagina, and small intestine. Prolapse of the bladder can also occur, but is dealt with by a urologist or urogynaecologist. Prolapse of the uterus can be treated by a gynaecologist, but if it is associated with rectal prolapse is dealt with by a colorectal surgeon.
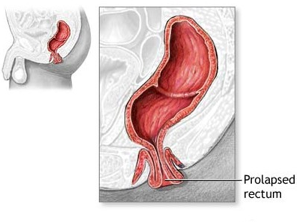
Rectal prolapse
The rectum is the final part of the large bowel, lying just above the anus. In women, the rectum and vagina are very close together but are normally kept separated by a strong wall of tissue known as the rectovaginal septum. If this tissue becomes weakened or damaged, the structures that keep the rectum in place begin to weaken such that the rectum can shift in position. In severe cases, the rectum can prolapse out of the vagina (a rectocoele), fall through the anus and be visible on the outside (external rectal prolapse), or telescope into the anus or another part of the rectum (internal rectal prolapse) without coming out of the anus.
Forty percent of women with a rectocoele have no symptoms. Those who do have symptoms may have difficulty controlling bowel movements, feel the need to have multiple bowel movements, and/or have a sensation of a bulge or fullness in the vagina. Occasionally, tissue may protrude out of the vagina.
An internal rectal prolapse often causes obstructive defaecation syndrome, ie, a sensation of a blockage in the bowel and difficulty passing a motion, with prolonged and often unsuccessful toilet visits. These patients frequently need to apply pressure with a finger or hand on the perineum, in the vagina, or on the anus to empty the bowel. Men with an internal rectal prolapse develop similar symptoms.
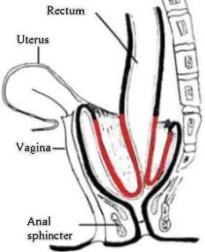
Investigations to exclude other causes will include a vaginal and rectal examination to assess the strength of the anterior (front facing) wall of the rectum. A special X-ray, called a defecogram, can also be used to evaluate the effect of the prolapse on bowel movements.
Rectal prolapse tends to occur gradually. Initially, the prolapse comes down with a bowel movement and then returns to its normal position. Rectal prolapse may be hard to distinguish from haemorrhoidal disease, and can be a confusing condition for specialists who are not evaluating and treating this problem on a regular basis.
Women over 50 years of age are six times more likely to develop rectal prolapse than men. It was thought historically that men do not suffer from pelvic organ prolapse because the male pelvis is much narrower than the female pelvis and does not need to deliver a baby. However, pelvic floor experts now recognise that men can also develop pelvic floor dysfunction. Most women with rectal prolapse are in their 60s, while the few men who develop prolapse are much younger, typically not more than 40 years of age.
Small bowel prolapse
In women, prolapse of the small (upper) bowel occurs when part of the small bowel prolapses into the upper part of the back wall of the vagina, creating a bulge (known as an enterocoele). Symptoms of an enterocoele may include a sensation of pelvic pressure and a feeling of blockage when going to the toilet. In women, an enterocoele is generally felt as a bulge into the vagina. The prolapse itself is not felt and may be difficult to diagnose. In men, the rectum is normally kept separate from the bladder in front of it by a strong wall of tissue known as the rectovesical septum. However, when the pouch between these structures is deep and there is pelvic floor dysfunction, a portion of small bowel may prolapse into this space, causing symptoms similar to those in women.
Surgical options
In women, rectocoeles and enterocoeles are usually defects of the tissue that supports the pelvis and not a problem with the bowel wall itself, so they are often treated by surgery that strengthens the back wall of the vagina.
There are a number of surgical procedures that can be performed for pelvic organ dysfunction. These include:
- Transanal rectocoele repair, an open procedure via the anus to repair a rectocoele. This is an option in patients who have symptoms from a rectocele and wish to avoid or cannot have abdominal surgery. It is lower risk, but there is a higher chance of the procedure not working.
- Rectoanal repair, an open procedure via the anus to repair a rectocoele or an internal rectal prolapse. This is useful in patients with some residual symptoms after a major robotic repair. It is also useful for those patients with less intrusive symptoms.
- Delorme’s procedure, an open procedure via the anus to repair an external rectal prolapse. This is generally reserved for less fit patients with short prolapses.
- Perineal rectosigmoidectomy (also known as Altemeier’s procedure), an open procedure via the perineum to repair an external rectal prolapse. This is generally reserved for less fit patients.
- Ventral mesh rectopexy and variations on this, ie, sacrocolporectopexyand modified Orr-Loygue rectopexy are laparoscopic or robotic procedures performed via the lower abdomen. Ventral mesh rectopexy and its variants are useful for repairing a rectocoele, enterocoele, internal rectal prolapse with obstructive defaecation syndrome or faecal incontinence, external rectal prolapse, or a vaginal prolapse. This is the treatment of choice for these problems.
Clearly, the choice of procedure depends on a number of factors, including the cause of your prolapse, your age, whether or not you have plans to start a family, and any other health problems you might have. All these issues will be discussed with you in detail when deciding on the type of repair that would be best for you.
For more information on Pelvic Organ Prolapse, please visit www.pelvicphysiotherapy.com

