- Abscess Incision and Drainage
- Advancement Flap Repair
- Anal Bulking
- Anal Tattooing
- Botulinum Toxin Injection
- Colectomy
- Delorme’s Procedure
- ELAPE Procedure
- Femoral Hernia Repair
- Fistulotomy
- Haemorrhoidectomy
- HALO-RAR Procedure
- Inguinal Hernia Repair
- Intersphincteric APR
- Lateral Internal Sphincterotomy
- Low Anterior Resection
- Pelvic Organ Prolapse
- Perineal Rectosigmoidectomy
- Rectoanal Repair
- Rubber Band Ligation
- Stapled Haemorrhoidopexy
- Stoma Creation
- Stoma Reversal
- Transanal Rectocoele Repair
- Umbilical Hernia Repair
colectomy
The large bowel is the last part of the intestines. It receives the end products of digestion and absorbs most of the remaining fluid and forms faeces. The large bowel consists of the colon and rectum. A colectomy, also known as a bowel resection, is a surgical procedure to remove all or part of your colon, and is used to treat several diseases of the colon, including inflammatory bowel disease, diverticular disease, and cancer. The type of colectomy performed depends on which part of the colon is affected by disease.
- Total colectomy – removal of the entire colon, leaving the rectal portion of the large bowel behind (for ulcerative colitis, Crohn’s disease, and in certain circumstances, bowel cancer).
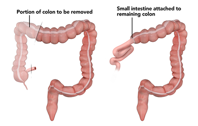
- Partial colectomy – removal of part of the colon (usually for bowel cancer or diverticular disease), including:
- - right hemicolectomy, where the right side of the colon (caecum, ascending colon and part of the transverse colon) is removed
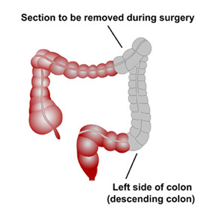
- - left hemicolectomy, where the left side of the colon (descending colon and sigmoid colon) is removed
- - sigmoid colectomy, where the sigmoid colon (last part of the colon) is removed.
- - right hemicolectomy, where the right side of the colon (caecum, ascending colon and part of the transverse colon) is removed
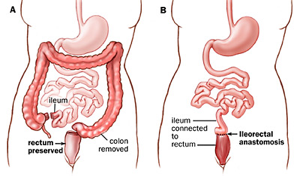
- Proctocolectomy – removal of both the entire colon and rectum (generally for ulcerative colitis, Crohn’s disease, and in certain circumstances, bowel cancer).
- When the colectomy has been performed, the remaining parts of your digestive system are reconnected to allow waste to leave the body. There are three ways in which this may be done:
- The remaining portions of your colon may be sewn or stapled together, creating a join called an anastomosis. Stool then leaves your body via the anus as before.
- Your colon (colostomy) or small intestine (ileostomy) may be connected to an opening made on the outside skin of your abdomen. This allows waste to exit your body through the opening (stoma). You may wear a bag on the outside of the stoma to collect faeces. This could be permanent or temporary.
- Your small bowel may be connected to your anus if you have had both your colon and rectum removed. A portion of your small bowel may be used to create a pouch that is then connected to your anus (ileoanal anastomosis). As part of this procedure, you may undergo a temporary ileostomy. This is only used for ulcerative colitis.
You will have the opportunity to discuss fully all the risks and benefits of your surgery with me before signing your consent form.
How a colectomy is done
In nearly all cases, a colectomy is planned as a laparoscopic (keyhole) procedure. The operation is performed using instruments inserted through three or more small cuts on your abdomen.All of these cuts are about 1–1.5 cm long, but one cut is longer because the diseased portion of bowel needs to be brought through to the outside of the body and removed without damaging the rest of the bowel. Exactly where these cuts are made depends on which portion of the bowel needs to be removed. A small video camera is passed through one of the cuts so that the inside of the abdomen can be seen on a TV monitor, and special surgical tools are passed through the other cuts to free the colon from the surrounding tissue. Carbon dioxide gas is used to inflate the abdomen slowly and give a clearer view of the bowel.
There are many delicate structures next to the colon that need to be protected and this is achieved by precision surgery. The blood vessels to the bowel are sealed and cut by special surgical instruments so the amount of blood loss is minimal. Once free, the portion of colon that needs to be excised is brought out through the abdominal wall. When the diseased part of the bowel has been removed, the remaining bowel ends can be joined together. A stoma is rarely needed. However, if the surgeon decides that safety may be compromised without a stoma, it will be formed at this stage.
A surgical drain is sometimes placed near the anastomosis. This is a thin tube that comes through the abdominal wall to the outside. As a last step, the wounds are closed with dissolvable stitches, followed by application of surgical glue that makes the wounds watertight.
You will be given a long-acting antibiotic in the anaesthetic room and an injection of local anaesthetic before you leave the operating theatre. The whole surgical procedure takes 1–4 hours, depending on complexity and patient factors. Right-sided colectomies generally take less time to perform than left-sided ones.
Very occasionally, a colectomy needs to done as an openprocedure. This involves making a single long (20 cm) incision on the abdomen to access the colon and using surgical tools directly to free the colon from the surrounding tissue and cut out either a portion of the colon or the entire colon. Again, the procedure takes 1–4 hours, depending on complexity and patient factors.
Nearly all non-emergency operations can be performed laparoscopically. An open approach is needed in 50% of cases if the colectomy is performed as an emergency. Further, there is a 5% chance of a colectomy that starts as a laparoscopic procedure needing to be switched to an open one. This is most likely to occur in patients who are obese and in those who have an obstructed bowel or adhesions from previous surgery.
A colectomy is always performed under general anaesthesia, so you will be asleep and feel no pain. You will be admitted to hospital on the day of your surgery and will need to fast from midnight on the night before if your surgery is scheduled for the morning or from 7 am if it is scheduled for the afternoon.
Full bowel preparation at home will be needed if you are having a left hemicolectomy, high anterior resection, or total colectomy. This entails you taking a special laxative to clear your bowel completely on the day before your surgery. You will receive detailed instructions on how to do this before your procedure. Preparation may also include a low-fibre diet. The following website explains in detail what you can eat on a low-fibre diet (www1.ghc.org/html/public/specialties/gastroenterology/colon-diet). You will be given detailed instructions on how to do this and the medication needed in advance of your admission. No bowel preparation is needed for a right hemicolectomy.
After your operation
After your surgery, you will be taken to the recovery area and then to the ward. When you wake up, you will have several tubes attached to your body, including an intravenous infusion tube in your arm to give you fluids and any necessary drugs, a catheter in your bladder to drain urine, and a drainage tube coming from the operation site to remove any oozing fluid. Most or all of these tubes are removed after 2–3 days. Supplementary oxygen is given by nasal prongs. Antibiotics are not generally necessary after a colectomy, but are given in some circumstances, particularly if the surgery has been performed as an emergency.
Some discomfort is common after surgery when your local anaesthetic wears off. The anaesthetist will decide on the method of postoperative pain relief that is best for you. Oral painkillers are all that is needed in most patients, but some require intravenous analgesia and a small number need an epidural. An epidural is often useful in emergency surgery where an open operation has been performed. It is rarely needed for laparoscopic surgery. Intravenous analgesia can be provided by a patient-controlled analgesia device, where a drip in your arm is connected to a syringe of pain-killing medication within a box. When the patient presses a button, a small dose of medication is pushed into the drip. There is a lockout that make it impossible to overdose. When you are discharged, you will be given pain medication to take home.
You can eat and drink as you wish after the operation, and if there is no problem with drinking, the drip providing fluid will be stopped. Some patients feel a little nauseous after eating and drinking soon after their surgery. In these patients, we wait a little longer before introducing food and fluids and keep the fluid drip going. You will be mobilised on the day following your surgery. The average stay in hospital after a colectomy is 3–5 days, but you may need to stay in longer if, for example, the join in the bowel leaks or the bowel is slow to start working again after surgery.
Many people find that their bowel function rapidly returns to normal and they can resume their normal diet immediately. Eating a balanced diet after your operation will aid your recovery. It is best to keep taking your analgesic medication until discomfort is manageable when going to the toilet. You may also be given medication to thicken or loosen your stools as needed.
You will not be able to drive when you are discharged from hospital, so it is important to arrange a friend or relative to take you home. When patients can resume driving after this type of surgery is determined on a case-by-case basis. This is usually 2 weeks, but will be discussed with you after your surgery. Most people need longer before they can safely, forcefully and quickly press the emergency footbrake to avoid a potential incident whilst driving. Please let your insurance company know when you have been given the all-clear to resume driving.
When you get home
Many people feel tired and weak after major surgery of this type, and full recovery may take up to 2 months. When you get home, you will need someone to help with meals, housework, and shopping. For the first week or two you may tire easily, so try to alternate short periods of light activity and rest in bed, taking care not to spend too much time lying down because of the risk of developing a blood clot in your legs (deep venous thrombosis).
Do not lift anything heavy, such as children, groceries or washing, or do strenuous work like digging the garden or lawn mowing for the first 6 weeks. You may resume intercourse when you wish.
You may get some pain off and on around your wound for several months, especially as you start to move and exercise more. This is to be expected. Taking a mild painkiller regularly will help with this. If the pain does not seem to improve or you are worried, contact your GP or our colorectal nurses.
How soon you can return to work following this type of surgery depends on what type of work you do, and this will be discussed with you after your operation.
A laboratory report on the piece of bowel removed during your surgery will be available 1–2 weeks after your surgery. The results of this and any further treatment needed will be discussed with you at your next appointment, which will be 2 weeks after surgery. If you have any questions or concerns about your surgery, please contact my office.

